Association between Nontraditional Risk Factors and Calculated 10-Year Risk of Atherosclerotic Cardiovascular Disease in a Large General Population: Based on the Pars Cohort Study
Authors
Pooran Mohsenzadeh, Ali Ardekani, Hossein Poustchi, Zahra Mohammadi, Seyed Reza Abdipour Mehrian, Hamed Bazrafshan Drissi, Zahra Rahimian, Erfan Taherifard, Ali Nabavizadeh, Alireza kamalipour, Bita Mesgarpour, Fatemeh Malekzadeh & Hossein Molavi Vardanjani
ABSTRACT
Background: While the traditional risk factors of atherosclerotic cardiovascular disease (ASCVD) have been well-established, the evolving role of nontraditional risk factors is not apparent. This study aimed to evaluate the association between nontraditional risk factors and the calculated 10-year ASCVD risk in a general population.
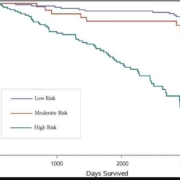
Methods: This cross-sectional study was conducted using the Pars Cohort Study data. All inhabitants of the Valashahr district in southern Iran, aged 40–75 years, were invited (2012-2014). Patients with a history of cardiovascular disease (CVD) were excluded. The demographic and lifestyle data were collected using a validated questionnaire. Multinomial logistic regression analysis was used to evaluate the association between the calculated 10-year ASCVD risk and the nontraditional risk factors of CVD, including marital status, ethnicity, educational level, tobacco and opiate consumption, physical inactivity, and psychiatric disorders.
Results: Of 9264 participants (mean age =52.2±9.0 y; 45.8% male), 7152 patients met the inclusion criteria. In total, 20.2%, 7.6%, 36.3%, 56.4%, and 46.2% of the population were cigarette smokers, opiate consumers, tobacco consumers, ethnically Fars, and illiterate, respectively. The prevalence rates of low, borderline, and intermediate-to-high 10-year ASCVD risks were 74.3%, 9.8%, and 16.2%, respectively. In multinomial regression, anxiety (adjusted odds ratio [aOR], 0.58; P<0.001) was significantly associated with a lower ASCVD risk, whereas opiate consumption (aOR, 2.94; P<0.001) and illiteracy (aOR, 2.48; P<0.001) were significantly associated with a higher ASCVD risk.
Conclusion: Nontraditional risk factors are associated with the 10-year ASCVD risk and, thus, might be considered besides traditional ones for ASCVD in preventive medicine and health policies.